If you’re searching for sleep aids, you probably want a better night of sleep without feeling foggy, unsafe, or dependent on a pill. “Sleep aid” is a big umbrella that includes non-medication strategies, OTC sleep aids, natural sleep aids, and prescription sleep aids.
This guide is educational, not personal medical advice. If you’re pregnant, over 65, have breathing problems, or take other medicines that cause drowsiness, it’s safest to ask a clinician or pharmacist first. Liftyolife aims to provide clear, safety-first health information you can actually use.
What you’ll learn:
- What counts as a sleep aid (and what doesn’t)
- What to try first for falling asleep vs staying asleep
- Side effects, interactions, and who should avoid specific options
- A comparison table and a screenshot-friendly safe-use checklist
What are sleep aids?
Sleep aids are tools that may help you fall asleep faster, stay asleep longer, or adjust your sleep timing. They include behavioral approaches (like CBT-I), nonprescription medicines, dietary supplements (like melatonin for sleep), and prescription medications. They can ease symptoms short-term, but they don’t always treat the cause of ongoing insomnia.
Key takeaways: Sleep aids can be useful, but if sleep trouble is frequent and long-lasting, the safest plan usually focuses on habits, schedule, and underlying conditions, not just sedation.
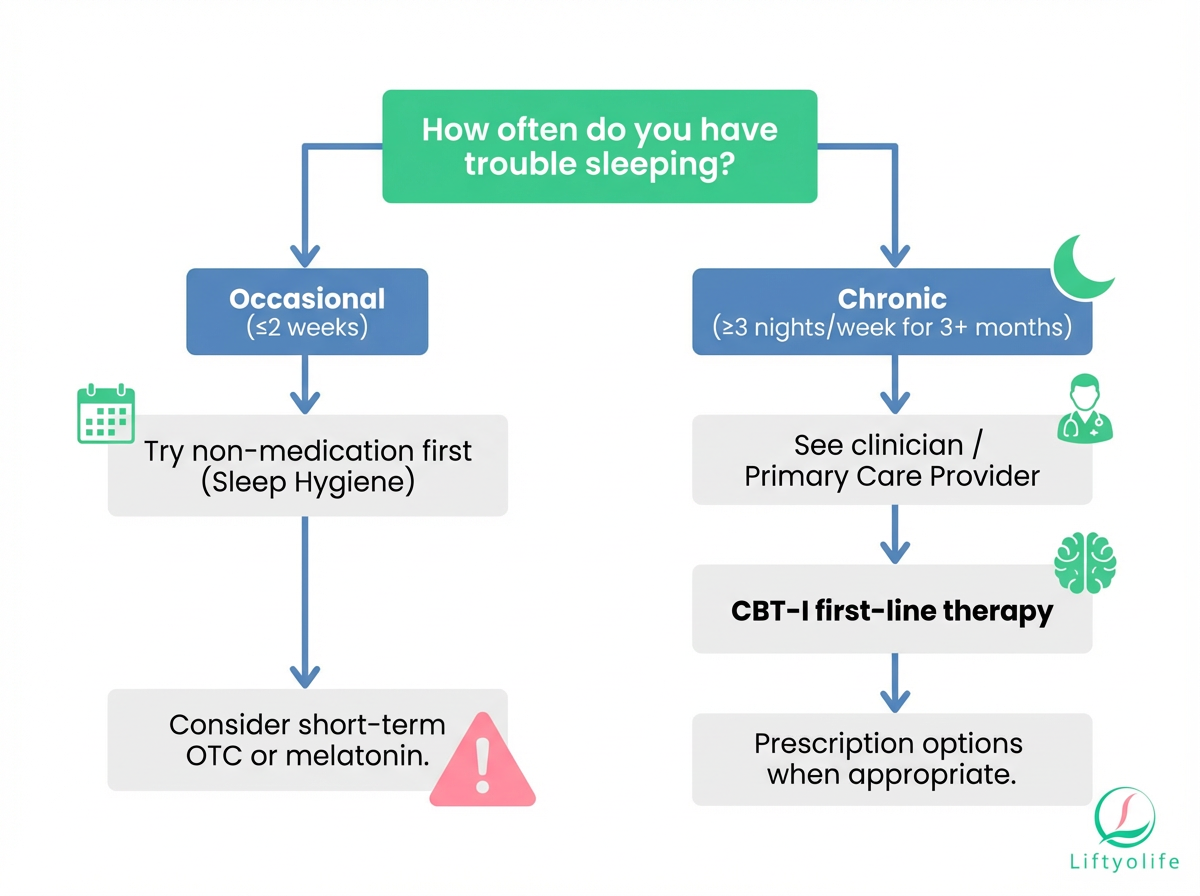
Sleep aids vs insomnia treatment
A few bad nights can happen to anyone during stress, travel, illness, or a schedule change. Chronic insomnia is different. It’s commonly defined as trouble sleeping at least 3 nights per week for 3 months or longer, plus daytime problems (fatigue, mood changes, poor focus).
For chronic insomnia, major guidelines recommend CBT-I (cognitive behavioral therapy for insomnia) as the first-line treatment because it improves sleep without the medication risks and tends to last longer than pill effects (American College of Physicians, American Academy of Sleep Medicine).
When sleeplessness can signal another issue
Sometimes sleep is the “messenger”, not the main problem. Consider a clinician evaluation if you also have:
- Loud snoring, gasping, or witnessed breathing pauses (possible sleep apnea)
- Uncomfortable leg sensations with an urge to move (possible restless legs syndrome)
- Persistent low mood, panic, or racing thoughts (anxiety or depression)
- A new medication that may disrupt sleep (for example, stimulants, steroids, some antidepressants)
Quick guide: choose a sleep aid by your problem
The best sleep aid depends on your main symptom and your risk factors. In general, start with non-medication steps first, then consider short-term OTC or supplements, and talk to a clinician for persistent insomnia.
- Trouble falling asleep: start with a consistent wake time + a wind-down routine + stimulus control; consider CBT-I; if your schedule is shifted (jet lag, shift work), melatonin may help with timing.
- Trouble staying asleep: prioritize CBT-I and sleep restriction therapy; check for contributors like pain, reflux, or sleep apnea; a clinician may discuss options like low-dose doxepin or a DORA in selected cases.
- Jet lag or shift work: use bright-light timing + melatonin for circadian timing; keep naps short and early.
- Stress-related short-term insomnia: relaxation training, journaling, and caffeine timing; if you use a medication, avoid alcohol and plan a full night in bed.
- Waking up too early: review alcohol timing, evening light, and too-early bedtimes; CBT-I can recalibrate your sleep window.
Safety guardrails that apply to almost all sleep aids:
- Don’t mix with alcohol.
- Only take a sleep aid when you can allow a full night of sleep.
- Don’t drive or operate machinery if you feel drowsy the next day.
Start here: non-medication sleep aids
Non-medication approaches are the safest starting point because they lower insomnia without creating tolerance, dependence, or next-day impairment. Even if you end up using a pill short-term, these steps often improve how well it works and make it easier to stop.
Sleep hygiene checklist
Use this as your baseline. Pick 2 tonight, not all 12 at once.
- Keep the same wake time every day, including weekends
- Get outdoor light within 1 hour of waking
- Stop caffeine 6 to 8 hours before bed
- Avoid alcohol within 3 hours of bedtime
- Keep the bedroom cool, dark, and quiet
- Use the bed for sleep and sex only. No email, scrolling, or work.
- Put screens away 60 minutes before bed
- If you nap, keep it 20 to 30 minutes and before mid-afternoon
- Exercise most days, but finish hard workouts 2 to 3 hours before bed
- If you’re awake about 20 minutes, get up and do something quiet, then return to bed when sleepy
- Keep late dinners and heavy snacks modest
- If worries spike at night, write tomorrow’s “next steps” before bed
If you want a deeper primer on routines and common sleep disruptors, see these practical tips on building a calming bedtime routine and avoiding sleep-disturbing behaviors.
CBT-I (cognitive behavioral therapy for insomnia)
CBT-I is a structured program that targets the thoughts and behaviors that keep insomnia going. It’s not “just therapy.” It’s skill-building, and it’s widely recommended as first-line care for chronic insomnia (ACP, AASM).
Common CBT-I components include:
- Stimulus control: retraining your brain to connect bed with sleep
- Sleep restriction therapy: narrowing time in bed to build sleep drive
- Cognitive strategies: reducing “If I don’t sleep, tomorrow is ruined” loops
- Sleep scheduling and education
Many programs run 4 to 8 sessions. You can access CBT-I through sleep clinics, some mental health clinicians, and validated digital programs.
Relaxation tools that can help tonight
These won’t “knock you out”, but they reduce hyperarousal so sleep can arrive more naturally.
- Box breathing: inhale 4, hold 4, exhale 4, hold 4 for 3 to 5 minutes
- Progressive muscle relaxation: tense then release muscle groups from toes to face
- Worry dump journaling: write the worry, then one next step
- Body scan: notice sensations, then gently return attention to breathing
OTC sleep aids (nonprescription medications)
Most OTC sleep aids in the U.S. are sedating antihistamines, usually diphenhydramine (a common diphenhydramine sleep aid ingredient) or doxylamine (a common doxylamine sleep aid ingredient). They can make you sleepy, but next-day impairment is common, and repeated use often works less well.
Antihistamines (diphenhydramine, doxylamine)
Best for: occasional, short-term sleeplessness when you can allow a full night in bed.
How it works: blocks histamine signaling (a “wakefulness” signal in the brain), but also has anticholinergic effects that drive many side effects.
Pros
- Easy to access
- Can cause sedation initially
Cons
- Next-day drowsiness and slower reaction time
- Dry mouth, constipation, blurred vision
- Confusion, especially in older adults
- Tolerance: the sleepy effect may fade with repeated use
Avoid if
- Age 65+ (the American Geriatrics Society Beers Criteria lists first-generation antihistamines as potentially inappropriate for many older adults due to anticholinergic burden)
- Glaucoma, BPH, or urinary retention risk
- You need to be alert early the next morning (driving, machinery, caregiving)
Safety tips
- Do not combine with alcohol, opioids, benzodiazepines, cannabis, or other sedatives unless a clinician specifically advises it
- Treat it like a short-term tool, not a nightly plan
- If you feel “hungover,” unsteady, or confused the next day, stop and reassess
Natural & supplement sleep aids
Natural sleep aids can feel “gentler”, but supplements are not regulated like prescription drugs. Product quality, labeling, and actual dose can vary. If you use supplements, choose conservative doses and look for third-party testing.
Melatonin
Best for: shifting sleep timing (jet lag, delayed sleep-wake phase, shift work) and occasional sleep-onset trouble tied to schedule disruption.
How it works: melatonin is a hormone your brain releases at night to signal “biological night.” Taking a small dose at the right time can help nudge your body clock.
Pros
- Generally well tolerated short-term
- Lower misuse potential than many sedatives
Cons
- Headache, nausea, vivid dreams, or next-day sleepiness in some people
- Too much or too late can worsen morning grogginess
Avoid if
- You’re pregnant or breastfeeding unless your clinician approves
- You take medications where interactions are possible (ask a pharmacist)
Safety tips
- According to the NIH Office of Dietary Supplements, common doses in practice are often 0.5 to 5 mg taken 1 to 2 hours before the target bedtime.
- More isn’t always better. Start low, and focus on timing.
Valerian
Best for: some people try it for mild, short-term sleep onset trouble, but research is mixed and effects are usually modest.
How it works: may have mild sedating effects through GABA-related pathways, depending on preparation and dose.
Pros
- Nonprescription option some people prefer
Cons
- Evidence is inconsistent and product-to-product variation is high
- Can cause drowsiness, headache, or stomach upset
Avoid if
- You take other sedatives or drink alcohol
- You’re pregnant or breastfeeding unless approved
Safety tips
- Don’t stack valerian with other sleep products
- Stop if you feel next-day impairment
Supplement quality & labeling
Before you buy a “sleep blend,” run this quick checklist:
- Look for third-party testing (USP, NSF, ConsumerLab)
- Avoid “mega-dose” labels unless a clinician advises it
- Check interactions (blood thinners, seizure meds, sedatives)
- Prefer single-ingredient products so you know what’s doing what
Prescription sleep aids
Prescription sleep aids are usually considered when insomnia is persistent, significantly affects daytime function, or when safer options like CBT-I are not enough on their own. Because risks vary by age, medical conditions, and other medications, these should be chosen and monitored with a clinician.
A good rule of thumb to discuss with your prescriber: use the lowest effective dose for the shortest effective time, with a plan to reassess.
DORAs (suvorexant, lemborexant, daridorexant)
Best for: sleep maintenance (staying asleep) and sometimes sleep onset in chronic insomnia.
How it works: DORAs block orexin, a wakefulness signal in the brain. Instead of broadly “sedating”, they reduce the wake drive.
Pros
- Helpful for staying asleep in many patients
- Lower dependence risk than benzodiazepines (still requires caution)
Cons
- Next-day sleepiness in some people (especially with higher doses or not enough time in bed)
- Vivid dreams or abnormal dreams
Avoid if
- You can’t allow a full night of sleep
- You use alcohol or other sedatives unless your clinician specifically manages the combination
Safety tips
- Review your full medication list with your prescriber, especially opioids and other CNS depressants
Z-drugs (zolpidem, zaleplon, eszopiclone)
Best for: short-term insomnia, often when rapid sleep onset is the main issue (exact fit varies by agent and formulation).
How it works: enhances GABA-A signaling to promote sedation.
Pros
- Often faster onset than behavioral tools
- Can be effective short-term for selected patients
Cons
- Next-day impairment, dizziness, and memory effects in some people
- The FDA requires a boxed warning for complex sleep behaviors (for example, sleepwalking or sleep-driving), which can cause serious injury
Avoid if
- You drink alcohol in the evening
- You’ve had complex sleep behaviors in the past
Safety tips
- Take only as prescribed and stop the medication and contact your clinician if unusual nighttime behaviors occur
Benzodiazepines (temazepam, triazolam)
Best for: selected cases, usually short-term, when benefits clearly outweigh risks.
How it works: increases GABA activity broadly, reducing arousal.
Pros
- Can reduce anxiety-related hyperarousal
Cons
- Higher risk of tolerance, dependence, and withdrawal
- Increased falls risk and cognitive impairment, especially in older adults
Avoid if
- History of substance use disorder (unless carefully managed by a clinician)
- You use opioids or have breathing disorders (unless closely supervised)
Safety tips
- Use the shortest effective duration and schedule follow-up to reassess
Other options (ramelteon, low-dose doxepin)
Ramelteon
- Best for: sleep onset, especially when abuse potential is a concern
- How it works: melatonin receptor agonist (targets melatonin receptors rather than acting as a sedative)
- Common downsides: dizziness, fatigue
Low-dose doxepin (3 to 6 mg)
- Best for: sleep maintenance, fix waking up during the night
- How it works: at low doses, it mainly blocks histamine signaling with less of the broad antidepressant effects
- Common downsides: next-day sleepiness in some people
Comparison table: common sleep aids at a glance
Choosing among sleep aids is less about “strongest” and more about matching the option to your sleep problem and risk profile. The tables below simplify evidence levels and risks to help you have a clearer conversation with a clinician or pharmacist.
Table 1 — OTC vs natural vs prescription vs CBT-I
| Option | Best for | Onset | Next-day impairment | Key risks | Avoid if | Evidence |
|---|---|---|---|---|---|---|
| CBT-I | Chronic insomnia | Slow (weeks) | None | Time, effort | Complex mental health needs* | High |
| Sleep hygiene | Mild, situational | Moderate | None | Low effect alone | N/A | Mod |
| OTC antihistamines | Occasional use | Fast | Common | Anticholinergic, falls | 65+, glaucoma/BPH | Low-Mod |
| Melatonin | Jet lag, circadian | Moderate | Sometimes | Grogginess, quality | Pregnancy (unless ok) | Mod |
| Valerian | Mild sleep onset | Moderate | Sometimes | Variable products | With sedatives/alcohol | Low |
| DORAs | Staying asleep | Moderate | Possible | Sleepiness, dreams | Alcohol, sedatives | Mod |
| Z-drugs | Mostly falling asleep | Fast | Possible | Complex behaviors | Alcohol use | Mod |
| Benzodiazepines | Selected cases | Fast | Common | Dependence, falls | Opioids, SUD history | Mod |
| Ramelteon | Sleep onset | Moderate | Low | Dizziness | Severe liver disease | Low-Mod |
| Low-dose doxepin | Sleep maintenance | Moderate | Possible | Sleepiness | MAOI use | Mod |
Evidence levels are simplified. Your age, medical history, and other medications can change what’s safest, so use these tables as a starting point for a clinician or pharmacist conversation.
Safety: side effects, interactions, and who should avoid
Side effects of sleep aids range from mild grogginess to serious problems like falls, breathing issues, or unsafe behaviors during sleep. The safest approach is to think in layers: 1) what you take, 2) what you mix it with, and 3) what your body is already dealing with.
Dangerous combinations (alcohol, opioids, sedatives)
If you take any medicine that slows the nervous system, check with a pharmacist before adding a sleep aid.
- Avoid combining sleep aids with alcohol. Alcohol amplifies sedation and worsens coordination.
- Opioids + sedatives can increase the risk of respiratory depression and overdose (CDC).
- Combining multiple sedating meds (benzodiazepines, Z-drugs, antihistamines) can raise the risk of falls, confusion, and dangerous impairment.
Older adults (65+)
Older adults tend to be more sensitive to sedation, and medicines often last longer in the body. That raises fall risk and confusion risk.
- OTC antihistamine sleep aids are often a poor fit because of anticholinergic effects (AGS Beers Criteria).
- Discuss CBT-I first, and ask whether safer medication choices exist for your situation.
- Reduce fall risk: use night lights, clear pathways, and avoid taking sedatives if you might need to get up often.
Pregnancy and breastfeeding
If you’re pregnant or breastfeeding, avoid self-prescribing sleep aids.
- Start with non-medication steps (routine, CBT-I, relaxation).
- Ask your OB-GYN, midwife, or clinician before using melatonin, valerian, or any sedating medication.
Medical conditions that change what’s safe
Some health issues make certain sleep aids riskier:
- Glaucoma/BPH/urinary retention: avoid anticholinergic antihistamines
- Breathing disorders (sleep apnea, COPD): sedatives can worsen nighttime breathing
- Depression or suicidality: some sedatives can worsen mood or be dangerous if misused
How to use sleep aids more safely
Screenshot this checklist if you want a quick reminder:
- Start with non-medication steps (routine, light, caffeine timing)
- Use the lowest effective amount for the shortest time
- Only take a sleep aid when you can allow 7 to 8 hours in bed
- Don’t mix sleep aids with alcohol
- Don’t “stack” multiple sleep products (for example, antihistamine + melatonin)
- Take it right before bed (not earlier in the evening)
- If you wake up unsteady, sit first and turn on a light
- Plan next-day safety: don’t drive if you feel impaired
- Reassess after 3 to 7 nights: needing it often is a signal to get help
- Store medications away from children and teens
When to see a doctor (and when it’s urgent)
If sleep problems happen 3+ nights per week and last 3+ months, or you’re regularly impaired at work, school, or while driving, talk with a clinician. You may have chronic insomnia that responds best to CBT-I, or another condition that needs targeted treatment.
Get evaluated sooner if you have loud snoring, choking or gasping, witnessed pauses in breathing (possible sleep apnea), or if you need sleep aids most nights to function.
Red flags that need urgent help:
- Thoughts of self-harm or suicide
- Severe chest pain, shortness of breath, or confusion
- A severe allergic reaction (swelling, widespread rash, trouble breathing)
- Sleepwalking or sleep-driving episodes after taking a sleep medication
Frequently Asked Questions
What is the safest sleep aid?
For most people, behavioral options, especially CBT-I, are the safest long-term approach because they improve sleep without medication side effects. Some OTC or supplement options can help short-term, but risks vary by age, health, and other meds. If you’re older, pregnant, or take sedating medicines, ask a clinician or pharmacist first.
What sleep aid works the fastest?
Fast options are typically sedating medications, but they can also cause next-day drowsiness and unsafe impairment. The best choice depends on whether you can allow a full night of sleep and your health conditions. Avoid mixing any sleep aid with alcohol.
Can I take diphenhydramine (Benadryl) every night?
It’s generally not intended for nightly, long-term use as a sleep aid. Risks include next-day drowsiness, confusion, constipation or urinary retention, and falls, especially in adults 65+. If insomnia is frequent, talk with a clinician about CBT-I and safer options.
Is melatonin safe for long-term use?
Many people tolerate melatonin, but long-term safety data is limited and product quality can vary by brand. Timing and dose matter, and higher doses aren’t always better. If you have a chronic condition, are pregnant, or take other medicines, ask a clinician or pharmacist first.
Which sleep aids are safest for older adults?
Older adults are more sensitive to next-day sedation and falls. OTC antihistamine sleep aids are often a poor fit because of anticholinergic effects. A clinician can help prioritize CBT-I and consider safer medication options when needed.
When should I see a doctor about insomnia?
If symptoms last 3+ months, happen 3+ nights/week, or impair daytime function, see a clinician. Get evaluated sooner if you have loud snoring or breathing pauses, severe daytime sleepiness, or if you rely on sleep aids regularly. Those can signal sleep apnea or another treatable condition.
Conclusion
Sleep aids can help in the short term, but the safest foundation is usually sleep habits and CBT-I, especially when insomnia is persistent. If you do use OTC, supplement, or prescription options, match them to your specific problem, avoid risky combinations like alcohol, and reassess quickly if you’re needing them often.
References
- Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline From the American College of Physicians – Recommends CBT-I as initial treatment.
- American Academy of Sleep Medicine: Behavioral and Psychological Treatments for Chronic Insomnia – Guideline summary.
- NIH Office of Dietary Supplements: Melatonin Fact Sheet – Evidence, dosing considerations, safety.
- NIH Office of Dietary Supplements: Valerian Fact Sheet – Evidence and safety cautions.
- FDA: Boxed warning for serious injuries caused by sleepwalking with certain prescription insomnia medicines – Safety warning for complex sleep behaviors.
- American Geriatrics Society Beers Criteria – Medication safety framework for older adults.
- CDC: Overdose Prevention – Opioid overdose risk and respiratory depression education.
- Sleep Foundation: Cognitive Behavioral Therapy for Insomnia (CBT-I) – Patient-friendly overview and what to expect.
- Harvard Medical School Division of Sleep Medicine – Sleep health education resources.