- What stress does to cortisol, hunger hormones, and your daily “energy budget”
- Why stress weight gain often shows up as belly fat
- A realistic 7-step plan you can start today (plus when to see a doctor)
If you’re stressed and gaining weight, you’re not imagining it
Work pressure, caregiving, money worries, health stuff, relationship stress. For many adults 35+, stress is not a short season. It is the background noise of life. And when that noise gets loud, routines slip: sleep gets shorter, meals get more random, and workouts either disappear or turn into punishment.
If the scale is creeping up, it’s easy to blame yourself. But stress weight gain is often driven by biology plus behavior: your body’s stress response can change appetite, cravings, sleep, and daily movement. That combination can add body fat over time, often around the midsection.
- You’ll learn the real (non-hype) link between stress and fat gain
- You’ll see why “cortisol belly” is a thing, but rarely the whole story
- You’ll get a simple plan for what to do today, this week, and this month
Do stress make you fat? Quick answer
Yes. Chronic stress can contribute to weight gain by increasing cortisol and nudging your habits in the same direction: stronger cravings (especially for sugar, salt, and high-fat “comfort foods”), worse sleep, and less everyday movement. Over weeks and months, those small shifts can add up to fat gain, often around the belly.
Most common pathways:
- Cravings and stress eating: your brain seeks quick comfort and reward
- Sleep loss: hunger hormones shift and impulse control drops
- Lower NEAT: you sit more and move less without noticing
Important: Stress affects people differently. Some people lose weight under stress, especially in the short term.
What stress does inside your body: cortisol, hunger hormones, and your “energy budget”
Cortisol in 1 sentence: Cortisol is a hormone that helps you handle demands, but when it stays elevated too often, it can push appetite, sleep, and fat storage in an unhelpful direction.
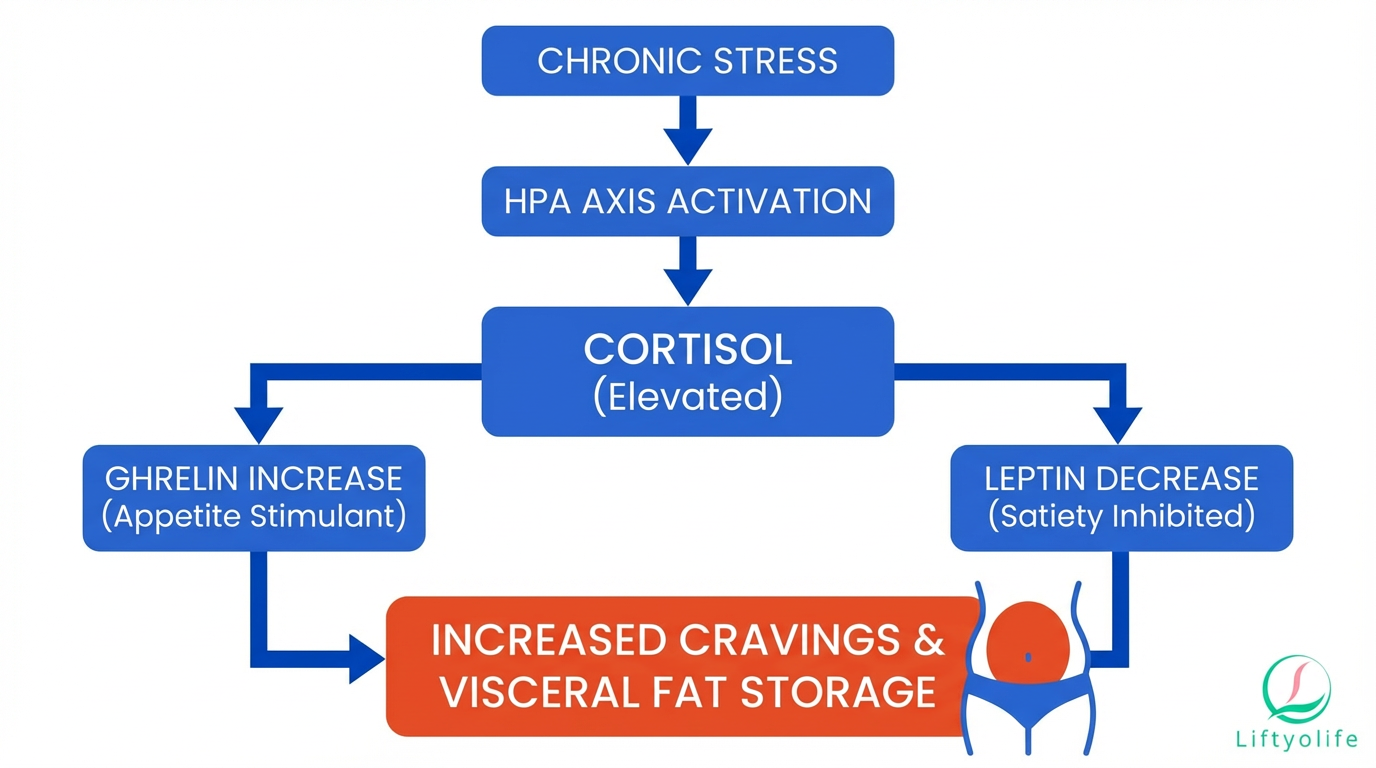
Cortisol and the HPA axis
Your stress system is often described as the HPA axis (hypothalamic-pituitary-adrenal axis). Think of it like a survival switchboard. When your brain senses a threat, it signals your adrenal glands to release cortisol so you have fuel, focus, and energy to respond.
In a true emergency, this is protective. In modern life, the “threat” might be emails, deadlines, caregiving, conflict, or being on-call 24/7.
Acute vs chronic stress: why the timeline matters
Acute stress (minutes to hours) can temporarily reduce appetite for some people. Chronic stress (weeks to months) is different: repeated stress signals can disrupt cortisol rhythms and make it easier to eat more, sleep less, and store fat centrally. Research reviews link chronic stress exposure with greater abdominal (visceral) fat in susceptible individuals (see PubMed review in References).
Your “energy budget”: appetite, blood sugar, and invisible movement
Weight change is rarely about one lever. Under chronic stress, several systems can shift at once:
- Ghrelin and leptin (hunger and fullness signals) can tilt toward “eat more” (PubMed).
- Insulin and blood sugar swings can raise cravings, especially if meals are irregular or ultra-processed foods become the default.
- NEAT (non-exercise activity thermogenesis) can drop. That’s the “invisible” calorie burn from walking around, cleaning, doing errands, standing, and even fidgeting. When you’re stressed and tired, you often sit more without realizing it.
How stress leads to weight gain (the 5 most common pathways)
- Cravings + stress eating
Stress can push you toward fast reward: ultra-processed snacks, sugary treats, or alcohol. These choices are easy calories, and they can also train the brain to use food as a coping tool.
Try this today: Build a “pause” before snacks. Drink water and wait 5 minutes. - Sleep disruption
Poor sleep is linked to changes in appetite regulation and makes late-night snacking more likely. When you’re exhausted, your brain also has a harder time choosing the slower, healthier option.
Try this today: Set a hard wake-up time for the next 7 days. - Lower daily movement (NEAT)
Stress often means more screen time and less casual movement. Even if you still do workouts, fewer steps and less standing can reduce daily calorie burn.
Try this today: Take a 10-minute walk after one meal. - Insulin resistance & blood sugar swings
Stress can worsen blood sugar volatility, especially paired with poor sleep and more refined carbs. Spikes and crashes can feel like sudden hunger and “I need sugar now” cravings.
Try this today: Add protein to your next snack (Greek yogurt, eggs, tuna). - Training stress / overexercising
Trying to “out-train” stress can backfire. Under-recovery can raise fatigue, increase appetite, and make workouts harder to stick with. The goal is steady training you can recover from.
Try this today: Swap one intense session for an easy walk or gentle cardio.
The stress – fat loop: why weight gain can increase stress
Weight gain can raise stress too, which is why this problem can feel sticky. You might feel self-conscious, avoid social plans, or get trapped in strict dieting during the week and rebound eating on weekends. Physiologically, higher abdominal fat is linked with inflammation, and it can worsen sleep quality for some people (for example, via higher sleep apnea risk).
This is a loop, not a personal failure. The goal is to change the inputs that keep the loop spinning.
| Loop accelerators | Loop breakers |
|---|---|
| Shame, self-criticism | Regular meals with protein/fiber |
| All-or-nothing dieting | “Good enough” consistency |
| Late-night scrolling | 10-minute wind-down routine |
| Skipping meals then grazing | Protein-forward breakfast |
| Alcohol to “take the edge off” | Planned alcohol boundaries |
| Sitting all day | 2×10-minute walks |
Table: Acute vs chronic stress – what changes
Chronic stress tends to drive stress weight gain because it changes your baseline: your sleep, appetite signals, and daily movement patterns. Reviews in obesity research describe how repeated HPA-axis activation and glucocorticoid exposure are associated with central fat accumulation in susceptible people (PubMed; PMC review in References).
Table: Acute vs chronic stress effects
| Factor | Acute stress (minutes–hours) | Chronic stress (weeks–months) |
|---|---|---|
| Cortisol pattern | Short spike | Repeated elevation/dysregulation |
| Appetite | Often lower at first | Often higher; more snacking |
| Cravings | Variable | More sugar/salt/fat cravings |
| Sleep | One bad night | Ongoing poor sleep quality |
| Movement (NEAT) | Unchanged | Often lower; more sitting |
| Fat storage | Minimal | More visceral/abdominal tendency |
Stress belly vs medical causes: when it’s more than stress
Stress can contribute to belly fat. But some weight changes have medical or medication-related drivers. If your gain is rapid, unexplained, or comes with other symptoms, it’s worth getting checked.
Not all cortisol is the same: stress vs Cushing’s
Everyday stress does not usually create the cortisol levels seen in Cushing syndrome. Cushing’s is a medical condition of chronic glucocorticoid excess (sometimes from taking steroid medication, sometimes from the body producing too much cortisol).
Red flags to ask about:
- Easy bruising or thin skin
- Wide purple stretch marks – striae
- New or worsening high blood pressure or blood sugar
- Proximal muscle weakness – hard to climb stairs or get up from a chair
- Rounder face and more central weight gain
Red flags: If you have several of the signs above or rapid unexplained weight gain, book a clinician visit. You are not being dramatic. You are being smart.
Other common reasons the scale moves
- Hypothyroidism: fatigue, cold intolerance, constipation, hair/skin changes
- PCOS: irregular periods, acne, excess hair growth, insulin resistance
- Menopause/andropause: body composition shifts, sleep disruption, less muscle
- Medications: systemic steroids, some antidepressants, antipsychotics, some seizure and diabetes medications (ask your prescriber, do not stop meds abruptly)
When to see a doctor
- Rapid gain (about 10+ lb in a month) without an obvious change
- Swelling in legs/face, shortness of breath, or chest symptoms
- Severe fatigue, weakness, or new mood symptoms
- Snoring, gasping, or suspected sleep apnea
- You started or changed a medication and weight jumped
- You’re unsure and want a basic screen
Break the cycle without burning out: the habits that lower stress AND help fat loss
You don’t need a perfect routine. You need a few defaults that make stressed days look more like your “healthy” days.
If you want more detail on how stress and cortisol can affect abdominal fat patterns, see our guide on reducing daily stress for weight management.
Sleep first
Why it helps: Sleep loss can shift appetite signals, increase cravings, and make workouts feel harder. It also lowers NEAT because you move less when you’re tired.
Do this today: Get 10 minutes of outdoor light within an hour of waking.
Food that stabilizes cravings
Why it helps: Regular meals with protein + fiber reduce blood sugar swings and lower the odds of grazing. They also make it easier to stop at “enough.”
Do this today: Aim for 25–35 g protein at your next meal (chicken, tofu, Greek yogurt, beans plus a lean protein).
Stress-snack list, pick what suits you:
- Greek yogurt + berries
- Apple + peanut butter
- String cheese + grapes
- Baby carrots + hummus
- Tuna packet + whole-grain crackers
Mini stress-proof grocery list:
- Protein: eggs, rotisserie chicken, canned tuna/salmon, tofu
- Fiber: frozen veggies, salad kits, beans, oats, berries
- Easy carbs: microwave rice, potatoes, whole-grain bread
- Flavor: salsa, olive oil, spices, pickles
Movement that calms the nervous system
Why it helps: Walking and light strength training can reduce stress reactivity for many people and help protect muscle while you lose fat.
Do this today: Do 2×10 minutes of walking, one earlier in the day and one after dinner.
Caffeine & alcohol boundaries
Why it helps: Late caffeine can wreck sleep. Alcohol can increase night waking and next-day cravings, even if it helps you fall asleep faster.
Do this today: Set a caffeine cutoff: 8 hours before bedtime.
Mental tools
Why it helps: If food is your main stress tool, you need at least one non-food option that works fast.
Do this today: Try 2 minutes of slow breathing: inhale 4 seconds, exhale 6 seconds.
If stress is driving emotional eating specifically, you may also like our practical reminders on healthy ways to cope with emotional eating triggers.
Time required: 10–30 minutes/day, plus two short strength sessions per week.
- Track stress + sleep + snacks for 7 days
Write down bedtime/wake time, stress level (1–10), and any snacks. No calorie counting. The point is to spot patterns you can change without shame. - Upgrade breakfast (protein + fiber)
A stronger breakfast reduces late-day cravings. Think eggs + fruit, Greek yogurt + oats, or tofu scramble + veggies. - Walk 20–30 minutes daily, or 2×10 minutes
This boosts NEAT and helps downshift your nervous system. If you can only do one thing this week, do the walk. - Do a 10-minute wind-down nightly
Dim lights, put your phone away, and repeat the same routine. The goal is consistency, not perfect sleep. - Set a caffeine cutoff + an alcohol rule
Pick a realistic cutoff time and keep alcohol to planned days only. Less decision fatigue means more follow-through. - Strength train 2×/week with a gentle start and avoid overtraining
Two full-body sessions help protect muscle and support insulin sensitivity. Start with 20–30 minutes and leave 2–3 reps “in the tank.” - Review results and choose your next support
After 2 weeks, look for better sleep, fewer cravings, and more steps. If weight is rising fast or symptoms suggest a medical cause, book a visit. If stress feels unmanageable, consider therapy or coaching support.
If you want a simple worksheet, use the Liftyolife stress-eating tracker (free printable) to log stress, sleep, and snacks for one week.
What to expect in 2 weeks:
- Fewer evening cravings
- More stable energy
- Possible drop in bloating or water retention (not always fat yet)
Stress weight gain vs other common causes
Many things can move the scale at once. This table helps you decide what to address first and when medical input matters.
Table: Common causes of weight gain (scroll on mobile)
| Cause | Clues you’ll notice | What helps first | See a clinician? |
|---|---|---|---|
| Stress overload | cravings, poor sleep | sleep + walks | if persistent |
| Sleep deprivation | late hunger, fatigue | fixed wake time | if snoring/gasping |
| Medication effect | change after new med | medication review | yes |
| Hypothyroidism | cold, constipation | labs + treatment | yes |
| PCOS | irregular periods | insulin support habits | yes |
| Simple overeating | larger portions | meal structure | if stuck |
Frequently asked questions
Can stress make you gain weight even if you eat the same?
- Yes. Stress can reduce sleep quality and daily movement (NEAT), lowering calorie burn even if meals look similar.
- Cortisol can increase water retention and may shift fat storage toward the abdomen.
- Track sleep, steps, and snacking for 7 days to spot small drift.
Why does stress fat go to my belly?
- Chronic cortisol exposure is linked with higher visceral (abdominal) fat in research.
- Belly fat is hormonally active and can be sensitive to sleep loss, inflammation, and insulin changes.
- Genetics, age, and menopause/andropause can amplify the pattern.
Can stress make you lose weight instead of gain?
- Yes. Some people eat less, feel nauseated, or move more when anxious.
- Acute stress can suppress appetite temporarily. Chronic stress more often disrupts sleep and cravings.
- Persistent unintentional weight loss should be medically evaluated.
- Many people notice appetite and sleep improvements in 1–2 weeks of consistent stress management.
- Visible waist changes often take 6–12+ weeks, depending on diet, activity, and hormones.
- Consistency beats intensity. Avoid all-or-nothing cycles.
- The term is informal, but the idea is grounded: chronic stress is associated with abdominal fat gain in research.
- It is rarely cortisol alone. Sleep, food choices, alcohol, and inactivity usually co-drive it.
- If you have classic Cushing’s signs (easy bruising, purple stretch marks, muscle weakness), see a clinician.
When should I see a doctor for stress weight gain?
- If weight gain is rapid (for example, 10+ lb in a month) or comes with swelling, shortness of breath, or severe fatigue.
- If you suspect medication side effects (steroids, some antidepressants).
- If you have red flags for hormonal disorders (Cushing’s, thyroid issues, PCOS).
Summary: what to remember
- Chronic stress can lead to weight gain through cravings, sleep loss, and lower NEAT.
- “Cortisol belly” is a real pattern in research, but it is usually multi-factor.
- The fastest wins are often: a fixed wake time, protein-forward meals, and daily walking.
- Overexercising can backfire if recovery is poor.
- Rapid or unexplained gain deserves a medical check.
Next best step:
- If sleep is the issue: start with a consistent wake time and a 10-minute wind-down.
- If cravings are the issue: add protein and fiber to breakfast and snacks.
- If symptoms feel “off”: schedule a basic medical review and medication check.
Small repeatable actions beat big perfect plans. If you change the inputs for two weeks, the loop starts to loosen.
Chronic stress can nudge your body toward belly fat by raising cortisol, disrupting sleep, and increasing cravings while lowering everyday movement. The fix is rarely extreme dieting; it is a few consistent habits that stabilize sleep, food choices, and activity, plus medical evaluation when weight gain is rapid or unexplained.
References + medical review
Last updated: 2025-12-18
- Stress and Obesity: Are There More Susceptible Individuals? – Review of stress, HPA axis, and obesity susceptibility.
- Chronic Stress Burden, Visceral Adipose Tissue, and Adiposity-related Inflammation – Human data linking stress burden to visceral fat and inflammation.
- Cleveland Clinic: Stress and Weight Gain – Clinician-reviewed overview of pathways and tips.
- Orlando Health: How Too Much Stress Can Cause Weight Gain (and what to do) – Practical clinical guidance.
- Mayo Clinic: Stress symptoms and management – Stress effects and management basics.
Disclaimer: If you have rapid weight gain, signs of hormonal disease, or symptoms like swelling or shortness of breath, seek medical care promptly.